Its victims include the actor Christopher Reeve, Pope John Paul II, and the British poet Rupert Brooke, who died after a mosquito bite on his lip became infected. Sepsis remains one of the leading killers in the United States and the world. Now, researchers describe a novel way to treat the lethal condition by filtering microbes from patients’ blood.
Sepsis is the body’s over-the-top reaction to an infection. Even with modern medical care, it can result in organ failure and death within just a few hours. Measures such as early treatment with broad-spectrum antibiotics—which slay many different kinds of bacteria—have reduced mortality in recent years, but no drugs specifically target sepsis. Cell biologist and bioengineer Donald Ingber of Harvard University and colleagues wanted to test a different therapy—a technique to pull microbes and the toxins they release from the blood. As their design guide, the researchers looked to the spleen; the organ filters out pathogens and poisons as blood wends through its narrow passages.
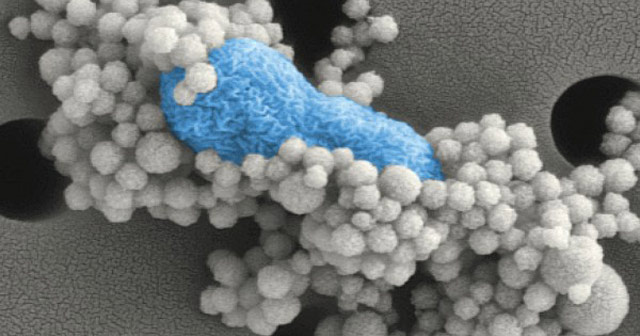
The team first needed a way to capture nasties. They coated tiny magnetic beads with fragments of a protein called mannose-binding lectin (MBL). In our bodies, MBL helps fight pathogens by latching onto them. Ingber and colleagues showed that the sticky beads could grab a variety of microbes in the test tube.
With that key challenge out of the way, the researchers were ready to design the rest of the system. They engineered a microchiplike device a little bigger than a deck of cards that works somewhat like a dialysis machine. As blood enters the device, it receives a dose of the magnetic beads, which snatch up bacteria, and then fans out into 16 channels. As the blood flows across the device, a magnet pulls the beads—and any microbes or toxins stuck to them—out of the blood, depositing them in nearby channels containing saline.
The researchers first tested their device with donated human blood tainted with bacteria. They found that filtering the blood through the device five times could eliminate 90% of the microbes.
Next, Ingber and his team hooked up anesthetized rats to a pump that circulated their blood across the device and then returned it to their bodies. After dosing the rats with bacteria, the researchers measured the effectiveness of their system. Within 1 hour, the device removed 90% of the microbes from the rats’ blood, the team reports online today in Nature Medicine.
To determine whether blood filtering improved survival, the researchers injected a lethal bacterial toxin into anesthetized rats and then used the device to filter the poison from the blood of some animals. Eighty-six percent of control rats died during the 5-hour experiment. If their blood was cleansed, however, only 11% of the animals perished. Although the beads don’t bind to all kinds of infectious microbes, “we get most bugs that are the most common causes of sepsis,” Ingber says. Moreover, because MBL attaches to an assortment of invaders, including viruses, the device could potentially remove pathogens that cause other diseases from the blood, including HIV and maybe even the Ebola virus, he says. It could also help treat illnesses triggered by abnormal blood proteins, such as autoimmune diseases.
“This is a very promising study using a very creative system,” says Richard Wenzel, an infectious disease specialist at Virginia Commonwealth University in Richmond.
But skeptics say it’s not clear whether the technique can be used for its intended purpose, treating sepsis. “What they’ve done is invent an artificial spleen,” says Clifford Deutschman, a critical care physician and sepsis researcher at the North Shore-Long Island Jewish-Hofstra School of Medicine in New Hyde Park, New York. He thinks the device could help many kinds of patients, including those with spleen injuries. But people with sepsis don’t usually have microbes or toxins in the blood, he says, so there may be nothing to remove.
Ingber disagrees. He notes that antibiotics often benefit sepsis patients, so reducing microbial numbers should be beneficial. “It’s got to help to pull out the bugs,” he says. He and his colleagues are planning to test the device in pigs, which more closely mimic human sepsis.
Source: AAAS
http://news.sciencemag.org/health/2014/09/artificial-spleen-could-help-treat-sepsis