HOW does cancer do it? How does one little cell transform itself into an invader that rages out of control? Surprisingly abruptly, according to new results that are pointing the way to Darwinian-inspired treatments.
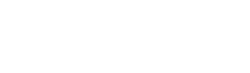
When a cancer evolves the ability to metastasise, or invade multiple tissues in the body, it has to pull off several remarkable feats: wrench itself from the primary tumour; thrive independently; burst through the wall of a blood or lymphatic vessel; outwit the immune system; and, finally, anchor and grow in a new location. Once it figures out how to do all this and can spread around the body, a person is unlikely to survive more than a few months.
Now Charles Swanton from Cancer Research UK and his team at University College London think they understand what happens. Rather than gradually collecting many tiny mutations, cancer dramatically reorders its genome, evolving these abilities in large leaps or "macromutations". This allows it to conjure up the suite of traits it needs to turn into a killer.
"Metastasis is an extremely complex process," Swanton says. "It's very unlikely that those multiple abilities can be driven by one gene."
Macromutation is an idea with a chequered past. In the 1940s, biologist Richard Goldschmidt argued that organisms splintered into new species when large mutations happen in a single generation, creating a well-adapted beast he called a "hopeful monster". His ideas were dismissed but the process has now been spotted in some plants and even animals, including flies and fish.
Cancer, Swanton says, evolves in an analogous way, lurching from benign tumour to metastatic disease just like Goldschmidt's hopeful monsters.
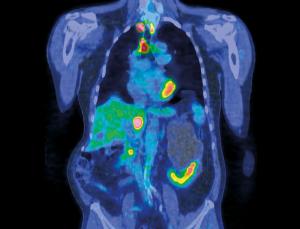
For 10 years we have known there is a connection between cancers with unstable chromosomes – ones prone to large mutations like gaining, losing or reordering chromosomes – and aggressive behaviour such as metastasis. But it wasn't clear if the instability was a cause of the aggression or a consequence. Now, armed with evidence from work on colon cancer cells, Swanton says it's a cause.
His group showed that cultured cells that had doubled their number of chromosomes during faulty cell division were better able to tolerate large-scale mutations. They could totally rearrange their genome, and continue living. In other words, the cells could become hopeful monsters (see diagram).
But this only shows that cancer cells can survive macromutations. Those mutations had to be linked to the evolution of deadly traits. So Swanton looked at what had happened to people whose cancer cells have doubled their genome. In 150 people with early colon cancer, genome doubling was associated with a fivefold increased risk of their cancer returning within two years of treatment. Together, Swanton says the results suggest genome-doubling could be a "macro-evolutionary leap" in tumours, which allows them to become killers (Cancer Discovery, doi.org/q29).
There are at least two ways that genome doubling could give cancer the impetus it needs. Swanton thinks genome-doubled cells could have acquired an earlier mutation that allows them to survive huge genomic rearrangements. That opens up an obvious treatment strategy: find that mutation and block it or reverse it.
Mutate and invade
Another possibility is that genome doubling itself buffers a cell, making it tolerant of mutations, says Giulia Rancati at the Agency for Science, Technology and Research in Singapore. Genome-doubled cells essentially have a back-up of every chromosome. So if one is deleted, moved, repeated or otherwise messed up, a healthy version can step in to lessen the overall impact of the change.
Rancati says the evidence for macromutation driving cancer evolution is overwhelming. "It suggests that cancer evolution does not happen by gradual accumulation of mutations but mutations that enable genome chaos," she says.
Last month, Fan Bai from Peking University in Beijing, China, and colleagues found intriguing hints that the key drivers of cancer's ability to spread might be some particular macromutations called copy number variations, where sections of chromosomes are deleted, moved or duplicated. In 11 people with lung cancer similar macromutations were repeated in each cancer cell, suggesting the mutations helped the cells survive or spread – possibly by driving metastasis (PNAS, doi.org/q3b). "Copy number variations could influence the functions of a large set of genes," says Bai. "Such changes could alter the gene expression of different pathways, conferring a selective advantage for metastasis."
Recognising that cancers evolve in giant leaps opens up new avenues for treatment. One might be to lower the rate that cells accumulate these macromutations. Evidence published last June by Carlo Maley from the University of California, San Francisco, suggested slowing the rate of copy number variations might be how aspirin helps prevent cancer.
This approach also suggests that chemotherapy may not help everyone. Although the drugs kill cancer cells, they also destablise the genomes of surviving cells, making chromosomal rearrangements more likely. Swanton says the effect could be to create more hopeful monsters. "I worry that you could you potentially make outcomes worse in a small population of patients," he says.
It's a balancing act, says David Thomas from the Garvan Institute in Sydney, Australia. Large mutations are very likely to kill a cell. Cancer needs to find an optimum level of mutation – the sweet spot between hopeful and hopeless monster. "There's a zone in the middle where there's a balance between being adaptable and being so genomically unstable as to compromise the cancer's success," he says.
The key will be to customise chemotherapy to push chromosomal instability past that sweet spot. Swanton's group is in the early stages of studying 3500 women with breast cancer to properly figure out what connects the degree of chromosomal instability, chemotherapy, and how well patients do. His team is carefully rating the chromosomal instability of tumours in all the women and will watch their progress through treatment.
If Swanton can find some key genetic changes in cancer cells that allow genome doubling and other macromutations, those could be targets for therapy that stops cancer from becoming deadly. That is a long way off. Even before new treatments emerge, a better understanding of cancer evolution might improve existing treatments and explain why some people initially respond to chemotherapy, only to see their cancer come back even more aggressively.
Source: New Scientist