People with Werner syndrome—a rare disease with symptoms that mimic premature aging—usually go gray in their 20s, develop cataracts and osteoporosis in their 30s, and die before 60. Now, researchers have for the first time created a key class of versatile stem cells that carry the genetic defect that causes the condition. Their analysis suggests that loosely wrapped DNA underlies the accelerated physical decline of Werner syndrome and promotes aging in the rest of the population.
Scientists have long sought to understand whether diseases such as Werner syndrome and Hutchinson-Gilford progeria syndrome (HGPS), in which children end up looking like old people and die by their teens, truly reflect accelerated aging. One approach has been to scrutinize patients’ stem cells, the unspecialized cells that spawn different types of tissues. Four years ago, for example, developmental biologist Juan Carlos Izpisua Belmonte of the Salk Institute for Biological Sciences in San Diego, California, and colleagues coaxed skin cells from HGPS patients to morph into one stem cell variety, so-called induced pluripotent stem (iPS) cells.
But when the researchers tried the same technique with cells from people with Werner syndrome, “it was tricky, and we were not able to do it,” Izpisua Belmonte says. The cells were too badly damaged to yield iPS cells. So the researchers went a different route. Because of mutations, the roughly one in 200,000 people who have the syndrome either lack the Werner protein (WRN), the jobs of which include copying and repairing DNA, or make a defective version of it. The team obtained stem cells from human embryos that had a normal WRN gene. Then they snipped two small segments from the gene, thus producing embryonic stem cells that are missing the Werner protein.
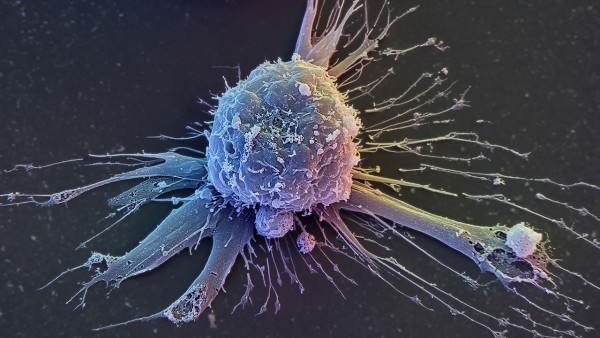
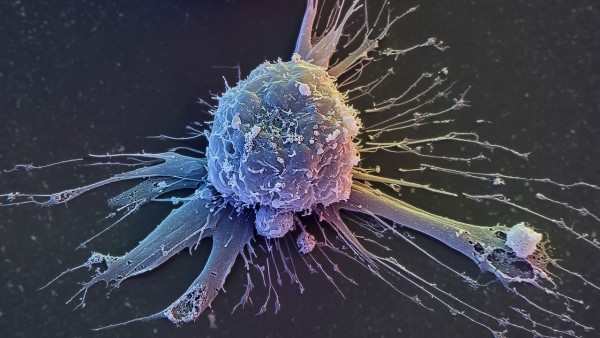
Embryonic stem (ES) cells can give rise to any type of cell in our bodies, and the ones the researchers created initially seemed normal. However, the symptoms of Werner syndrome suggest defects in patients’ mesenchymal stem cells (MSCs), a more specialized stem cell type that is the source of fat, cartilage, and bone cells. When the team induced the ES cells to mature into MSCs, the cells appeared to age rapidly. DNA damage—a hallmark of aging—was prevalent in the MSCs, for instance. They gradually lost the ability to divide and showed other signs they had entered a stagnant state known as cellular senescence, which might impair the ability of worn and damaged tissues to refurbish themselves. The MSCs also sported shorter-than-normal telomeres, which protect the tips of chromosomes. Many researchers think that deterioration of these structures contributes to aging.
Other studies have indicated that organisms alter how they package their DNA as they age. DNA doesn’t just float free. Our cells wrap their genetic material around proteins to form chromatin. Young, vigorous cells typically scrunch some of their chromatin into an orderly arrangement known as heterochromatin. Izpisua Belmonte and colleagues report online today in Science that the amount of heterochromatin in the stem cells declined.
The same thing happens in people who are aging normally, the researchers discovered. They tested MSCs from the teeth of six young people and six middle-aged and elderly folks, none of whom had Werner syndrome. The researchers found less heterochromatin in the older group, suggesting that their DNA had become disorganized with age.
“This study provides evidence that abnormal chromatin structure … is likely a major contributing factor to premature aging characteristic of the genetic disorder Werner syndrome,” says molecular biologist Robert Brosh of the National Institute on Aging in Bethesda, Maryland, who wasn’t connected to the research. In addition, he says, the work suggests that “defective chromatin organization may underlie normal aging as well.”
The research isn’t the first to implicate heterochromatin declines in premature aging conditions, says biochemist Lucio Comai of the University of Southern California in Los Angeles. However, “it reinforces the important concept of the role of chromatin in these diseases and in aging.”
If dwindling heterochromatin does drive aging, researchers still need to determine how. Cinching up DNA usually silences genes, and reducing the amount of heterochromatin in a cell could switch on genes that should be switched off, Izpisua Belmonte says. Heterochromatin also reins in transposable elements: segments of DNA that jump from place to place in our genomes. Comai notes that decreasing the amount of heterochromatin could unleash these restless strands, which can cause mutations with each move.
Source: AAAS, Full Article